Throughout 2020 and now into our second year of the COVID-19 pandemic, many people might be able to relate when saying the coronavirus “felt close to home.” Whether you have received a positive diagnosis personally or a loved one has been affected by COVID-19, when someone you know has a difficult experience with the virus, it can truly shape perspectives.
Our team is thankful to report that Sarah, a nurse here at Charleston Allergy & Asthma, is now farther along on her road to recovery than she was just a few months ago, but her experience with COVID-19 as a 37-year-old, healthy and active woman is not as uncommon as you would think.
We sat down with Sarah to learn more about her experience as a “long hauler” (the nickname given to those with prolonged cases of COVID-19), and how she fought along the road to recovery from the coronavirus.
When were you first diagnosed with COVID-19 and do you know how you may have contracted it?
I tested positive for COVID-19 on June 28, 2020. I’d recently gone in for a surgical procedure and had to be tested prior to that on June 23. I didn’t go anywhere prior to the surgery or after, so I assume that I contracted COVID during my hospital visit for the procedure. I began having symptoms on June 25.
What initial symptoms did you experience with COVID-19 and how did they progress over time?
- Day 1: extreme lower back pain, terrible headache.
- Day 2: sore throat, mild sinus congestion.
- Day 3: raw and sore throat, severe sinus congestion, loss of taste and smell.
- Day 7: intense sinus congestion, headaches and fatigue. Still no signs of fever, body aches or chills.
- Day 10: chest tightness, breathing issues, starting to really decline.
- 4 weeks: breathing under control, but now experiencing heart issues including heart palpitations and chest pain. Received EKG that came back abnormal and was referred to a cardiologist.
- Continued experiencing heart-related symptoms including an inconsistent heart rate. (i.e. Heart rate in the 140s while sitting and resting, 180s while standing, feeling short of breath, nearly passing out.)
- 5 weeks: diagnosed with tachycardia and began treatment for myocarditis (inflammation of the heart muscles).
- Also experienced a range of different symptoms in this time period, including hurting calf muscles, bloating, gas, heartburn, diarrhea, constipation and vomiting. Began to lose my hair in clumps, had extreme fatigue and felt “brain fog” (couldn’t remember words, had forgetful days, etc.) Felt like every nerve in my body was firing off at the same time, causing tremors. Taste and smell had only partially returned, certain foods tasted strange. Gained 30 pounds. Felt like every system in my body was failing.
- Eventually diagnosed with Dysautonomia; autonomic nervous system was damaged by COVID-19, which controls heart rate, blood pressure, breathing and digestion. Severely deconditioned by the time physical therapy was started and had no muscles in hips or legs.
What specific treatment did you seek in hopes of recovering from COVID-19?
I have seen our wonderful Dr. Moore at Charleston Allergy & Asthma since my initial diagnosis. I also consulted with a pulmonologist, cardiologist, gastroenterologist, neurologist and I have now been in physical therapy twice a week since the end of October. I received a wide variety of tests including chest x-rays, CT of the chest, EKG, ECHO, Holter monitor, cardiac MRI, endoscopy and colonoscopy. I’ve also been prescribed several medications including antibiotics, daily inhaled steroid, rescue inhaler, oral steroids, beta-blocker, colcrys, countless vitamins, turmeric, probiotics, peppermint oil pills and Pepcid.
Are you still receiving treatment for your COVID-19 symptoms?
I am still in physical therapy and follow up with my cardiologist and primary care provider every other month.
Are you still experiencing any lasting symptoms of COVID-19?
I still have heart rate issues, extreme fatigue, shortness of breath with exertion, headaches, brain fog and occasional GI issues.
How has COVID-19 affected your everyday life?
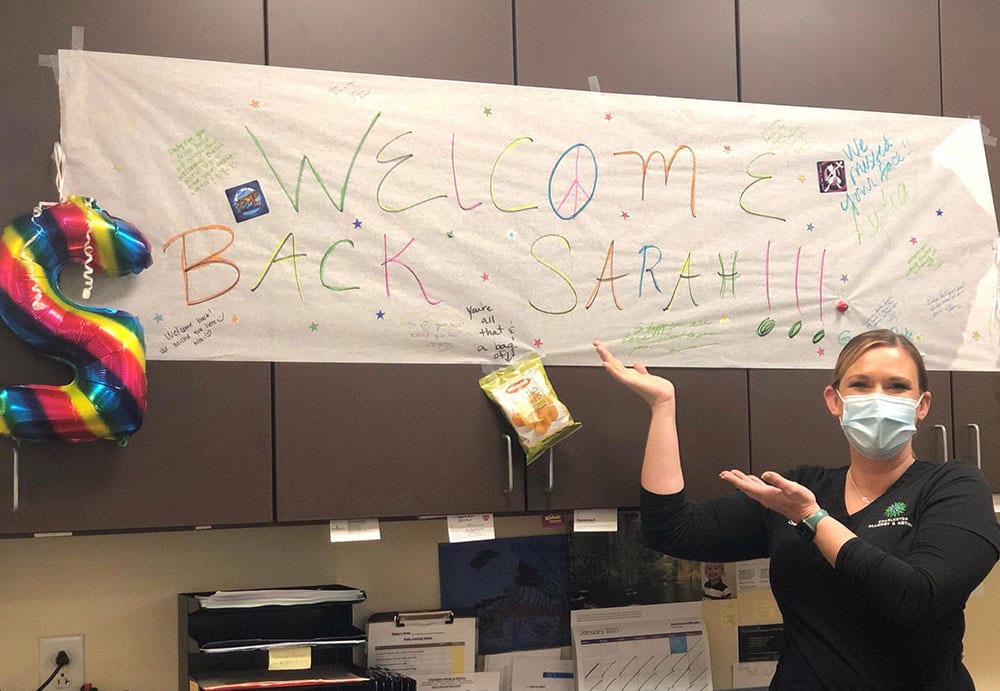
COVID-19 continues to have an extreme affect on my everyday life, even now as I’m many months post-diagnosis. I haven’t been able to work full-time in the office for over seven months. I’m fortunate my work has been so patient, as I have just started to return to the office occasionally, for a few hours at a time so I’m not pushing myself too hard. My work has made it possible for me to do some things from home so I can continue to have income. I haven’t been able to venture out anywhere, although we all should be staying home as much as possible to help reduce the spread of COVID-19 anyway. But I miss small, simple things, like going to the grocery store, picking up a coffee.
As I’ve started to feel better over time, I have experienced some exciting milestones. One big milestone was finally being able to clean my home on New Year’s Eve, it felt like such a big step after being bed ridden for so long. Who knew you could be so excited to clean your house?!
I’m incredibly grateful that Charleston Allergy & Asthma’s team has supported me throughout this journey. They have been super understanding if I’ve been unable to work or if I have a bad day. The people in my life, friends, family, co-workers, have had the greatest impact on my comfort and healing. There’s a big mental aspect to this disease and my support system has been incredible.
How are you currently seeking encouragement and support throughout your COVID-19 journey?

Early on into my diagnosis, I joined several Facebook support groups. After five weeks of being sick, I shared my story on Facebook and it went viral (pun intended) and was shared over 1,200 times all over the world. People were contacting me from New Zealand, Australia, Africa, Germany and throughout the U.S. I have honestly met people that I now consider friends or my “COVID sisters” as we joke, who are going through the same thing as me. My boyfriend, family and friends have been amazing and have helped me with so much. Plus, I am lucky to work from home right now and have also been able to do some self-care by reading books, binging shows, and even took up paint-by-numbers!
What encouragement do you have for those who have similar cases of COVID-19?
I think the biggest thing for people going through this is being your own biggest advocate. Doctors don’t know what causes these symptoms and you really have to fight for treatment and make sure your providers are listening to you. Most testing comes back normal which is frustrating, yet you have all these things going on in your system that can’t be explained. Also, be patient with the healing process. Early on, I knew that I was going to be in this for the long haul and tried my best to stay positive and not get discouraged when I had setbacks. Your mental attitude and fight toward this is everything.
Don’t underestimate COVID-19. Yes, a lot of people get through this illness, but sadly a lot of people have lost their lives. You truly do not know how your body will react. I was a healthy, active 37-year-old with no health issues and I had my life as I knew it stripped away from me. And, unfortunately, my case is not uncommon. There are thousands of people going through what I am going through and it just really is not talked about widely. We need our story to be heard so that more take notice and help figure out what is going on.
Sarah is still on the road of recovery from COVID-19 and continues to serve as an incredible member of the Charleston Allergy & Asthma team. She recently received her COVID-19 vaccinations along with the rest of the Charleston Allergy & Asthma staff and shares her story to help raise awareness of the potential affects the coronavirus can have on those diagnosed with the virus.



